Top 5 Healthcare Challenges in 2026 [+ Strategies to Mitigate Them]

The Top 5 Healthcare Challenges in 2026 are:
- Escalating Operational Costs
- Workforce Shortages and Burnout
- Cybersecurity Threats
- Technology Integration Challenges
- Financial Pressures and Ineffective Revenue Cycle Management
Operational costs are climbing faster than reimbursements. The workforce is stretched thin, and even the most seasoned staff are feeling the pressure. New technologies promise better outcomes but integrating them often feels like fitting puzzle pieces from different sets. Add cybersecurity risks and tight margins into the mix, and the day-to-day challenges can start to feel beyond overwhelming.
Sounds familiar? Healthcare executives across the U.S. are facing a perfect storm of rising expenses, talent shortages, digital complexity, and financial strain. And while there’s no single fix, there are smart, strategic steps you can take to regain control and build a more resilient operation in 2025 and the years ahead.
1. Escalating Operational Costs
Operational expenses are increasing. To paint a general picture:
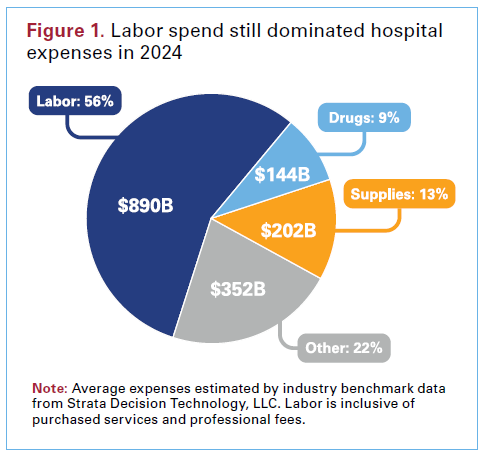
- Labor costs increased by over $42.5 billion between 2021 and 2024, totaling $839 billion and constituting nearly 60% of average hospital expenses.
- Medical supply expenses also rose to $146.9 billion in 2023, comprising about 10.5% of the average hospital’s budget, a $6.6 billion increase from the previous year.
2025 has been no different, and the trend indicates an even larger increase.
So, what can centers do to respond to escalating operational costs:
-
Optimize Key Processes
To tackle rising operational costs, healthcare organizations must prioritize process optimization across clinical and administrative workflows. For example, hospitals can streamline patient flow by identifying and removing bottlenecks in scheduling, admissions and discharge processes to help reduce unnecessary patient wait times and free up resources faster, directly impacting bottom-line performance.
-
Integrate Technology
Digital and AI-powered tools are no longer optional in today’s healthcare operations. Advanced technologies like AI tools to automate scheduling, real-time inventory tracking, and electronic health records (EHRs) reduces administrative overhead while improving accuracy and efficiency. For instance, predictive analytics can help forecast supply needs and reduce overstocking or emergency procurement costs. Over time, these tools contribute to measurable reductions in waste, duplicated efforts, and unnecessary expenditures.
-
Outsource Non-Core Functions
Outsourcing non-core functions such as revenue cycle management (RCM), medical billing, scheduling and transcription can dramatically cut operational costs while ensuring high levels of accuracy and compliance. Partnering with healthcare BPO providers offers access to experienced talent and scalable infrastructure without the overhead of in-house teams. This also allows internal teams to focus on core clinical and strategic initiatives, increasing institutional agility and overall patient service quality.
2. Workforce Shortages and Burnout
The healthcare industry faces critical staffing shortages, with an estimated 1 million nurses expected to retire between 2027 and 2030. Physician burnout has led to a significant exodus of healthcare professionals, with resignations growing by 50% between 2020 and 2024.
-
Retention Programs
High attrition is one of the costliest issues facing healthcare organizations today. Investing in career development programs, leadership training, and recognition systems improves morale and builds institutional loyalty. Strong retention strategies reduce the frequency and cost of recruiting new talent, while improving institutional knowledge continuity.
-
Cross-Training and Role Diversification
Rather than constantly hiring to fill gaps, cross-training existing staff to handle multiple roles improves organizational flexibility. This strategy also makes employees feel more empowered and valued, which strengthens retention. If you’re investing in this approach, it’s essential to understand the importance of proper healthcare staff training and how it ties directly to performance and patient outcomes.
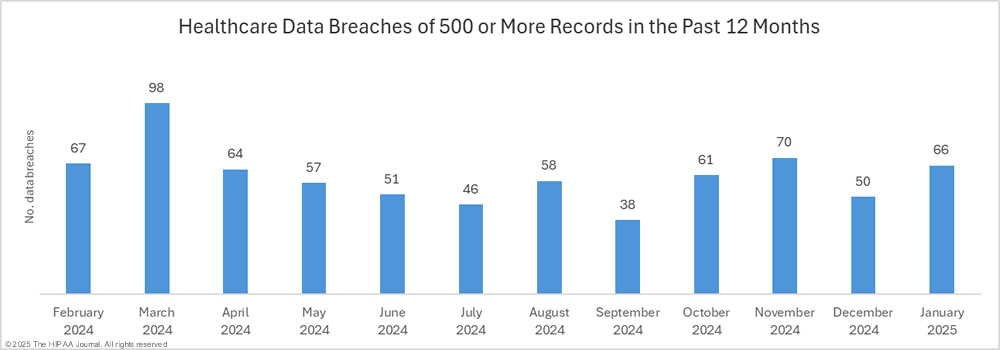
3. Cybersecurity Threats
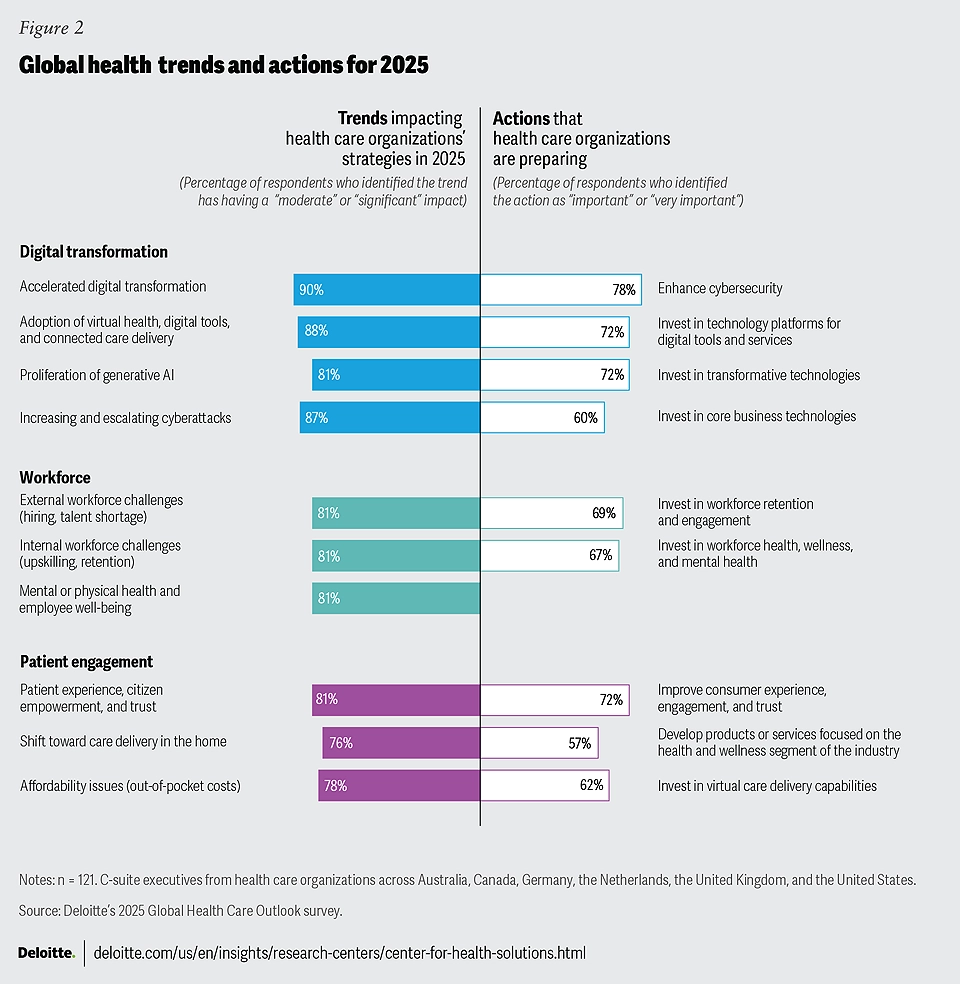
Healthcare organizations are increasingly targeted by cyberattacks, with the average cost of a single healthcare data breach reaching $9.77 million in 2024. Hospitals are expected to continue investing in cybersecurity measures to protect sensitive patient data and maintain operational integrity.
-
Robust Cybersecurity Measures
Data breaches continue to rise in frequency and cost. Implementing comprehensive security protocols, like encryption, multi-factor authentication, and regular penetration testing, is no longer just an IT priority. It’s a board-level issue. Cybersecurity must be embedded into the organizational culture to protect sensitive patient information and maintain trust.
-
Staff Training
Technology alone can’t stop cyber threats. Educating your entire workforce on phishing scams, password hygiene, and data handling policies is key to reducing human error. Ongoing education ensures that your people, not just your systems, are your first line of defense.
-
AI-Powered Threat Detection
Machine learning tools can proactively detect suspicious activity before it becomes a crisis. These systems analyze patterns and flag anomalies, allowing your IT team to act quickly and decisively. While this technology requires upfront investment, it dramatically reduces the risk of costly data breaches and system downtime.
4. Technology Integration Challenges
The fast advancement of healthcare technology presents integration challenges, with many organizations struggling to keep up with new systems and software. To avoid overwhelmed staff and operations, healthcare centers should prioritize key areas where technology can really make a positive change and speed up processes.
-
Interoperable Systems
Investing in interoperable EHR platforms ensures patient data can move seamlessly across departments and external partners. This not only supports better clinical decision-making but also boosts operational efficiency.
-
Cloud-Based Platforms
Cloud infrastructure offers greater scalability, enhanced security, and cost-effectiveness. These platforms also support remote care models and facilitate real-time collaboration between care teams. Cloud adoption has become a must-have for organizations aiming to modernize quickly without ballooning capital expenses.
-
Employee Training
Technology delivers ROI only when it’s used correctly. Without ongoing support, even the most advanced tools can lead to confusion or non-compliance. That’s why a structured staff training program is essential, particularly when rolling out new systems that impact patient care or administrative workflows.
5. Financial Pressures and Revenue Cycle Management
As reimbursement rates tighten and regulatory demands evolve, hospitals are struggling to maintain steady cash flow while handling complex billing processes. Denied claims rates going through the roof, underpayments, coding errors, and outdated systems continue to drain financial resources. On top of that, staffing shortages in billing departments and payer delays make it difficult to close the revenue loop efficiently.
What can centers do about it?
-
Value-Based Care Models
The transition from fee-for-service to value-based care helps shift focus toward outcomes, prevention, and patient engagement. These models reward efficiency and care quality rather than volume, leading to better patient experiences and long-term cost reduction. Adopting this model successfully requires internal alignment between clinical, financial, and operational teams.
-
Advanced Analytics
Predictive analytics helps finance leaders identify revenue leakage, track claim denials, and optimize payer mix strategies. With the right tools, CFOs can make real-time decisions that improve cash flow and enhance the accuracy of forecasting models.
-
Strategic Partnerships
Building alliances with external vendors and solution providers can bring in the expertise and scale that healthcare systems often lack internally. Partnering with a specialized healthcare call center can provide measurable financial and operational benefits. These partnerships also reduce fixed costs and introduce scalable support that adjusts to patient demand.
The healthcare challenges of 2026, from operational overload to workforce burnout, are complex but not impossible to overcome. Healthcare leaders who take a proactive, strategic approach can reduce costs, retain talent, and prepare their organizations for sustainable growth. It all starts with smarter investments, stronger partnerships, and a clear understanding of how every operational decision impacts both patient care and financial health.
If your organization is facing increasing operational strain or administrative overload, our healthcare BPO solutions can help. From revenue cycle management to contact center services, we offer scalable, HIPAA-compliant support designed to improve efficiency and reduce costs. Connect with us today to explore how we can help you streamline operations and achieve your performance goals.



