10 Strategies to Optimize Call Flows in Healthcare Centers

The top 10 Strategies to Optimize Call Flows in Healthcare Centers are:
- Implement a Secure, HIPAA-Compliant Call System with Smart Routing
- Minimize Patient Hold Times and Call Abandonment
- Train Staff to be Empathetic and Efficient
- Standardize Call Scripts and Scheduling Protocols
- Integrate Scheduling Systems for One-Touch Resolution
- Optimize Staffing for Peak Call Times
- Implement Call-Backs and Virtual Hold Technology
- Offer Self-Service Scheduling Options to Patients
- Track Key Call Center Metrics and Set Targets
- Conduct Quality Assurance and Continuous Improvement Assesments
For operations staff, chiefs of operations, and healthcare center managers, optimizing inbound calls isn’t just about speed—it’s about improving patient access and communication in a meaningful way. Despite the rise of online portals, a majority of patients still rely on the telephone for scheduling medical appointments. Nearly 90% of patients continue to book appointments by phone at least some of the time. This means that every missed call or minute on hold can directly impact patient satisfaction and even whether a patient receives timely care.
These 10 strategies provide actionable ways to streamline call flow processes in healthcare centers that will help reduce hold times, improve scheduling efficiency, and ensure each patient interaction over the phone is a positive experience.
1. Implement a Secure, HIPAA-Compliant Call System with Smart Routing
The foundation of an optimized call flow is a reliable phone system that meets healthcare’s privacy requirements. Ensure your call center software or phone system is HIPAA-compliant, meaning it safeguards patient information during call recording, voicemail, and data storage. Beyond compliance, leverage features like Interactive Voice Response (IVR) menus and smart call routing. An IVR can greet callers with a friendly automated menu (e.g., “Press 1 for appointments, Press 2 for prescription refills”) and quickly direct them to the appropriate department or agent.
Consider using skill-based routing, which connects the caller to an agent best suited for the patient’s needs. For example, calls about scheduling a cardiology appointment can automatically route to staff trained in that clinic’s scheduling protocols. By getting patients to the right person on the first try, you reduce unnecessary transfers and shorten the overall call handling time.
2. Minimize Patient Hold Times and Call Abandonment
Long wait times are a top complaint in healthcare call centers. To keep patients from hanging up in frustration, make reducing hold times a priority. Start by analyzing call volume patterns to staff appropriately: if Monday mornings have a call spike, ensure extra agents are available then. Set a goal for your team such as answering a high percentage of calls within a certain number of seconds (many call centers target answering 80% of calls within 30 seconds as a service level). This helps create a concrete benchmark for your staff.
Another effective tactic is implementing a call-back feature. This technology lets patients opt to receive a return call when an agent is free, rather than waiting on hold. It preserves their place in line without the frustration of listening to music. Providing an estimated wait time or position in the queue can also help manage expectations when holds are unavoidable.
The impact of these efforts is significant. In one survey, about 3% of patients admitted to hanging up without ever reaching a person due to extended waits.
3. Train Staff for Empathy and Efficiency
Even with great technology, the people answering the phones are critical to a smooth call flow. Comprehensive training should balance empathy with efficiency. Patients calling a healthcare center may be anxious, in pain, or confused about a medical issue. Agents need to convey compassion and patience, while still gathering information and handling the scheduling swiftly.
Provide customer service training that includes active listening, de-escalation techniques for upset callers, and clear communication. For instance, teach staff to politely interrupt long explanations with gentle questions that guide the call: “I understand, Mrs. Smith. Let me gather a few details so we can get you an appointment as soon as possible.” This way, the agent shows empathy but also keeps the conversation on track.
Also, train staff thoroughly on the scheduling software and electronic health record system so they can navigate it quickly during calls.
4. Standardize Call Scripts and Scheduling Protocols
Variation in how different agents handle calls can lead to inconsistent service. Creating standard call scripts and scheduling protocols ensures that every patient gets a reliable experience and no key step is missed. Develop a script for the call opening that includes a warm greeting and identification of the clinic or hospital, as well as asking for the caller’s name and reason for calling. For example: “Thank you for calling City Health Clinic, this is John. May I have your name and help you schedule an appointment today?”
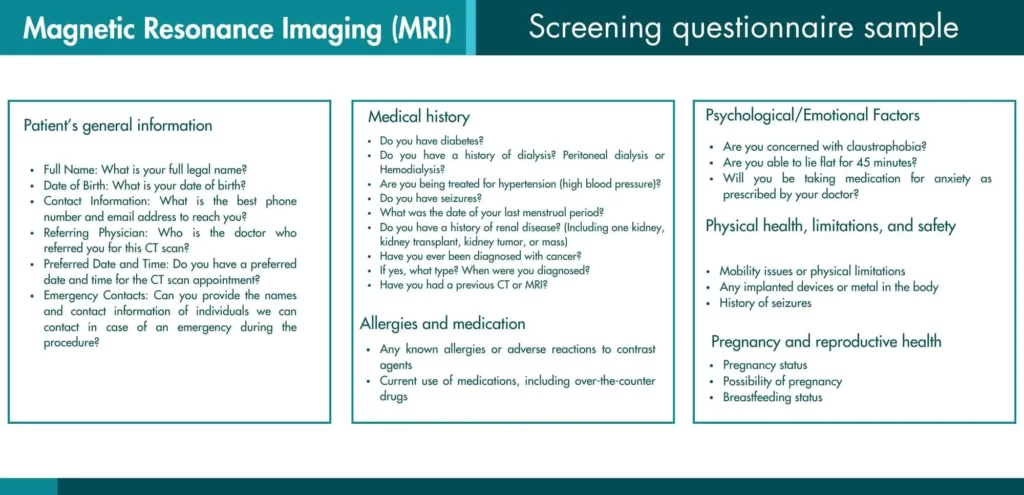
Beyond the greeting, use a checklist or template for the scheduling process. This should include all necessary information an agent must gather or provide during the call, such as:
- Patient details (full name, date of birth, contact information).
- Reason for the appointment or symptoms (to triage urgency or assign the right provider).
- Preferred times or dates and flexibility.
- Insurance information or referral details if applicable.
- Verifying the appointment date/time back to the patient and giving any special instructions (e.g., fasting requirements, arrival time, what documents to bring).
By standardizing these elements, you reduce errors and the need for call-backs because everything is handled in one call. It also helps new staff ramp up faster, since they have scripts to follow. Be sure to keep scripts conversational – agents should sound natural, not like robots reading a checklist. The script is a guide, but personal connection is still important.
5. Integrate Scheduling Systems for One-Touch Resolution
A frequent culprit of long call times is having to put callers on hold while staff check multiple systems or call a clinic to confirm an appointment slot. To optimize the call flow, integrate your call center software with your scheduling system and EHR (Electronic Health Record). When an agent can see real-time appointment availability on their screen and book it while the patient is on the line, it eliminates back-and-forth delays.
Integration might involve a unified dashboard where the incoming call triggers a “screen pop” with the caller’s information (if they’re a known patient and your system has caller ID integration). At minimum, the scheduling representatives should be working directly in the same scheduling software that the clinic uses. This way, booking an appointment over the phone is the same process as staff would do in person, ensuring no double-bookings or overlooked calendar updates.
For example, if a patient calls to schedule a follow-up with Dr. Lee, the agent should be able to see Dr. Lee’s calendar, offer open slots to the patient in real time, and lock in the appointment immediately. They should also be able to update patient contact info or insurance details in the record if needed, all without transferring the call. An integrated system speeds up calls and increases first-call resolution – the patient’s request is fully resolved by the end of the first call, with no need for a call-back or waiting for confirmation.
6. Optimize Staffing for Peak Call Times
Call volume in healthcare is not constant throughout the day or week. Use your phone system’s reporting or call analytics to identify peak call times – for many practices, early weekday mornings and the lunch hour are especially busy, as well as just after offices open on Mondays. Once you know when surges happen, schedule your staff accordingly. This could mean having more agents start work during the busy hours and slightly fewer during slow periods (like mid-afternoon or late evening).
Creating a coverage plan might involve staggered shifts. For instance, instead of all agents working 9–5, some might work 8–4 and others 10–6 to cover early and late-day spikes. Also, ensure your team takes breaks in rotations so that you don’t end up with multiple agents away at the same time when calls are pouring in. The goal is to have the right number of people on the phones at the right times.
Cross-training staff can provide flexibility too. If your front desk staff or billing team is trained to handle scheduling calls in a pinch, they can help field calls during an unexpected rush (and vice versa). From an operations perspective, this is about matching resources to demand as closely as possible. Adequate staffing during peaks will significantly cut down hold times and abandon rates, improving the patient experience during those crunch times.
7. Implement Call-Backs and Virtual Hold Technology
Sometimes high call volume is unavoidable, and patients may still end up in a queue. An advanced call flow strategy is to offer a virtual hold with a call-back option. Rather than asking patients to “please hold, your call is important to us” indefinitely, modern phone systems can assure the patient that the system will call them back as soon as it’s their turn. The patient can hang up and go about their day, and the system will automatically dial them back and connect to an agent when available.
This feature directly tackles the frustration of waiting on hold. Patients appreciate the convenience – they feel the clinic respects their time. Just be sure to set proper expectations: the system should inform them roughly when to expect the call-back (e.g., “in approximately 10 minutes”) and then deliver on that promise. Also, ensure that the call-back functionality is working smoothly; test it regularly so no call slips through the cracks.
Through call-backs, centers can lower the likelihood of abandoned calls. A patient who might hang up after 5 minutes on hold is less likely to be lost if they’ve opted for a call-back. This keeps your queue intact without wearing down your callers’ patience. It’s a win-win: the call center evens out the workload, and the patient isn’t tethered to their phone waiting.
8. Offer Self-Service Scheduling Options to Patients
While this article focuses on inbound calls, one way to improve call flow is to reduce unnecessary calls in the first place. Offering self-service appointment scheduling through online portals or mobile apps can offload routine calls from your staff. Many patients, especially younger demographics, appreciate the convenience of booking or cancelling appointments online without having to call at all.
For example, a health system might enable online scheduling for routine check-ups or vaccine appointments. If even 10–20% of patients start using online booking, that’s 10–20% fewer calls for your team to answer. Make sure to integrate the online system with your call center processes: agents should see appointments made online and not double-book over them.
Of course, not everything can or should be self-service. Complex appointments, surgical scheduling, or patients who have multiple questions will still prefer to call and speak to someone. The key is to use self-service for the simpler tasks so that your phone lines remain open and quick for those who truly need personal assistance. Always communicate clearly to patients about where to go for self-service and when they should call, so they choose the most efficient option for their needs.
9. Track Key Call Center Metrics and Set Targets
You can’t optimize what you don’t measure. Establishing and monitoring key performance indicators (KPIs) for your healthcare call center is essential to identify areas for improvement. Important metrics to track include:
- Average Speed to Answer (ASA): How quickly, on average, calls are answered by a live agent. A shorter ASA means patients spend less time waiting.
- Call Abandonment Rate: The percentage of callers who hang up before reaching an agent. Lowering this rate indicates more patients are getting through without frustration.
- Average Handle Time (AHT): How long an agent spends on each call, including hold time and after-call work. Efficient call flows aim to keep AHT reasonable without rushing the patient. Read 6 Ways to Improve Average Handle Time (AHT) at Outpatient Centers
- First Call Resolution (FCR): Whether the patient’s issue (scheduling the appointment, answering their question) was resolved on the first call, with no need for follow-up. High FCR is a sign of effective call handling.
- Patient Satisfaction Scores: If you conduct post-call surveys or track patient feedback, this qualitative metric is crucial for understanding the patient’s perspective on the scheduling experience.
Set clear targets for these KPIs based on industry benchmarks and your organization’s goals (for instance, an abandonment rate under 5% might be a target to strive for). Regularly review the metrics with your team. If ASA starts creeping up or abandon rates spike on certain days, investigate and address it – maybe staffing is short at a certain hour, or a new agent needs more training.
10. Conduct Quality Assurance and Continuous Improvement Assesments
Lastly, quality assurance (QA) practices help maintain a high standard of service on every call. Implement a routine of reviewing call recordings or side-by-side listening in on live calls. Use a QA scorecard to evaluate key aspects of the call: Did the agent follow the script and verify the caller’s identity? Did they display empathy and professionalism? Was the information provided accurate and complete? Scoring calls on these factors can highlight both individual training needs and systemic issues.
Share feedback with your team regularly. For example, you might have weekly coaching sessions where you play snippets of recorded calls (anonymized as needed) to illustrate great technique or areas to refine. Recognize agents who consistently handle calls well – it boosts morale and sets a positive example.
Additionally, solicit patient feedback. Look for comments about what caused any dissatisfaction – was it long hold times, confusing phone menus, or an agent who seemed rushed? Use this information to adjust your training, scripts, or processes. Continuous improvement means you iterate on your call flow: even after implementing these strategies, keep fine-tuning as you learn what works best for your patient population and staff.
Success in patient scheduling calls is measured not just by faster call times, but by happier patients who feel cared for and confident in their choice of your facility. A well-optimized call flow means a patient’s phone experience is smooth: calls are answered promptly, needs are addressed on first contact, and the process feels easy. For a healthcare organization, that translates to better operational efficiency, more filled appointments, and a strong reputation for patient-centered service that can only be achieved with continuous attention and improvement.
Streamline your healthcare center’s call flow, enhance patient communication, and boost scheduling efficiency.
Explore our healthcare call center solutions and discover how we can help you create a better patient experience from the very first call.